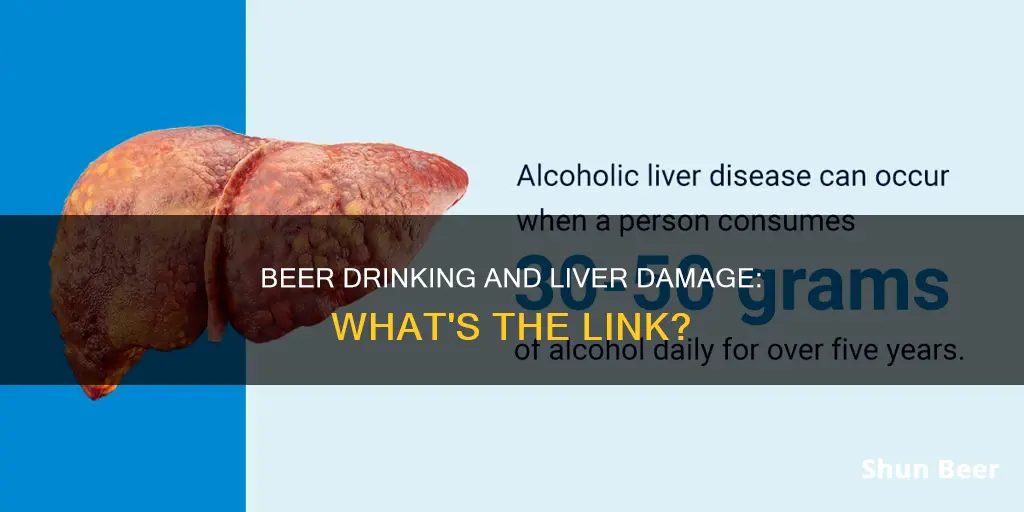
Alcoholic liver disease is a condition caused by alcohol abuse. The liver is an incredibly complex organ with a wide variety of functions, including filtering toxins from the blood and aiding digestion. Each time the liver filters alcohol, some of its cells die. While the liver can develop new cells, prolonged alcohol misuse over many years can reduce its ability to regenerate, leading to permanent damage. Alcoholic liver disease has three main stages: alcoholic fatty liver disease, alcoholic hepatitis, and cirrhosis. The condition is preventable and treatable if caught early, but it can be life-threatening if left untreated.
| Characteristics | Values |
|---|---|
| Liver disease caused by alcohol | Alcohol-related liver disease (ARLD) |
| Liver functions | Filtering toxins from the blood, aiding digestion of food, regulating blood sugar and cholesterol levels, helping fight infection and disease, producing bile that aids in digestion, converting vitamins, nutrients, and medicines into substances the body can use, storing glycogen for energy |
| Alcohol-related liver disease stages | Alcoholic fatty liver disease, Alcoholic hepatitis, Cirrhosis |
| Alcoholic fatty liver disease | Build-up of fats in the liver, caused by drinking a large amount of alcohol even for a few days |
| Alcoholic hepatitis | Inflammation of the liver, caused by alcohol misuse over a longer period or binge drinking; can be mild or severe |
| Cirrhosis | Significant scarring of the liver, caused by years of heavy drinking; irreversible and can lead to fatal liver failure or liver cancer |
| ARLD symptoms | Yellowing of the eyes and skin (jaundice), swelling in the ankles and tummy, confusion or drowsiness, vomiting blood or passing blood in stools |
| ARLD treatment | Abstinence from alcohol, preferably for life; liver transplant in severe cases |
| ARLD prevention | Stop drinking alcohol or stick to recommended limits, spread drinking over several days, have drink-free days |
What You'll Learn

Alcoholic fatty liver disease
The liver breaks down most of the alcohol an individual consumes, so it can be removed from the body. However, the process of breaking it down can generate harmful substances. These substances can damage liver cells, promote inflammation, and weaken the body's natural defences. The more alcohol that is consumed, the more the liver is damaged.
The risk of alcoholic fatty liver disease is higher for heavy drinkers who are female, obese, or have certain genetic mutations. Alcoholic fatty liver disease can lead to cirrhosis, which is the final phase of alcoholic liver disease. Cirrhosis is generally not reversible, but stopping drinking alcohol immediately can prevent further damage and significantly increase life expectancy.
The treatment for alcoholic fatty liver disease is to stop drinking alcohol. Abstinence from alcohol can restore normal liver function and allow individuals to return to a normal life.
Beer and Low-Fat Diets: Friends or Foes?
You may want to see also

Alcoholic hepatitis
The liver is a resilient organ capable of regenerating itself. However, each time the liver filters alcohol, some of its cells die. Prolonged alcohol misuse over many years can reduce the liver's ability to regenerate, resulting in serious and permanent liver damage. Alcoholic hepatitis is a potentially serious condition that can develop from alcohol misuse over a long period. It may be the first sign that a person is damaging their liver through alcohol consumption. Less commonly, alcoholic hepatitis can occur if a person consumes a large amount of alcohol in a short period (binge drinking).
The liver damage associated with mild alcoholic hepatitis is usually reversible if the person stops drinking permanently. However, severe alcoholic hepatitis is a serious and life-threatening illness. Many people die from this condition each year, and some people only discover their liver damage when it reaches this advanced stage. About one-third of heavy drinkers develop alcoholic hepatitis, where the liver becomes inflamed and swollen, and liver cells are destroyed. This condition varies in severity and can range from mild to severe. Patients may experience jaundice, fever, nausea, vomiting, and abdominal pain. The mild form can last for years and lead to more liver damage if the patient does not stop drinking. Severe alcoholic hepatitis occurs suddenly, usually after binge drinking, and can be life-threatening.
The treatment for alcoholic hepatitis involves abstinence from alcohol. For those with mild-moderate alcoholic hepatitis, abstinence, along with adequate nutritional support, remains the cornerstone of management. About 10% to 20% of patients with alcoholic hepatitis are likely to progress to cirrhosis annually, and 10% of individuals with alcoholic hepatitis experience a regression of liver injury with abstinence. For those with severe alcoholic hepatitis, specific treatment with corticosteroids or pentoxifylline medication may be used to reduce liver inflammation.
The Science of Beer Tubes: How Do They Work?
You may want to see also

Cirrhosis
The symptoms of cirrhosis include:
- Fatigue, weakness, and muscle wasting
- Increased pressure in the liver
- Accumulation of fluids in the abdomen and legs
- Bleeding from veins in the oesophagus
- Confusion, decreased concentration, and behavioural changes
The best treatment for cirrhosis is for the patient to stop drinking alcohol. Even if you've been a heavy drinker for many years, reducing or stopping your alcohol intake will have important short- and long-term benefits for your liver and overall health.
Beer and Bypass Surgery: What You Need to Know
You may want to see also

Alcohol-induced liver cancer
Alcohol consumption is a well-known cause of liver damage and liver cancer. Alcoholic liver disease (ALD) refers to liver damage and dysfunction caused by alcohol abuse. ALD can progress through several stages, from alcoholic fatty liver disease to alcoholic hepatitis and eventually cirrhosis, which is often irreversible.
Alcohol is classified as a Group 1 carcinogen by the International Agency for Research on Cancer due to its ability to induce hepatocellular carcinoma (HCC), the most common type of primary liver cancer. Heavy alcohol consumption is associated with a twofold increased risk of developing HCC. The risk is influenced by various factors, including the amount and duration of alcohol intake, gender, coexistence of viral hepatitis, and diabetes.
The mechanisms by which alcohol contributes to HCC development are not yet fully understood, but several pathways have been proposed:
- The mutagenic effects of acetaldehyde, a toxic metabolite of ethanol, which can damage DNA and proteins.
- Increased oxidative stress and reactive oxygen species (ROS) production, leading to lipid peroxidation and DNA damage.
- Impaired nutrient absorption and altered methylation patterns, affecting gene expression.
- Increased blood levels of estrogen, a hormone linked to breast cancer risk.
- Contaminants introduced during fermentation and production, such as nitrosamines and asbestos fibers.
Additionally, alcohol interacts with other factors like smoking, viral hepatitis, and diabetes, further elevating the risk of HCC.
The risk of HCC decreases by about 6-10% each year after stopping alcohol consumption, but it may take up to 23 years for the risk to approach that of non-drinkers. Surveillance and early detection are crucial, as curative treatments are more likely to be successful when HCC is identified early.
Beer and Diabetes: What Diabetics Need to Know
You may want to see also

Acute alcoholic hepatitis
Alcoholic liver disease is damage to the liver and its function due to alcohol abuse. Alcoholic hepatitis is an acute form of alcoholic liver disease (ALD) and is regarded as a specific clinical entity characterised by rapid decompensation of hepatic function. The disease spectrum of alcoholic hepatitis is wide, ranging from a subclinical form with good short-term outcomes to a severe acute illness associated with high mortality.
The exact incidence and prevalence of alcoholic hepatitis are unclear, as many patients have subclinical disease and are never diagnosed. However, one study reported the prevalence of alcoholic hepatitis in a cohort of 1604 alcoholics to be approximately 20% based on liver biopsy data. According to another study, alcoholic hepatitis accounted for 56,809 hospitalisations in the United States in 2007, with an overall inpatient mortality rate of 6.8%. Acute renal failure, infections, hepatic encephalopathy, coagulopathy, and ascites were strongly associated with mortality.
Alcoholic hepatitis has been linked to excessive alcohol drinking over a prolonged period, typically more than two decades. However, many patients diagnosed with alcoholic hepatitis report alcohol use over shorter periods. Heavy drinking is defined as 15 or more drinks per week for men and eight or more drinks per week for women. Binge drinking is defined as the consumption of five or more drinks by a male or four or more drinks by a female in about two hours, resulting in a blood alcohol concentration of 0.08% or higher. Binge drinking is a potential risk factor for alcoholic hepatitis and is thought to contribute to the rising incidence in younger individuals.
The diagnosis of alcoholic hepatitis is primarily based on clinical presentation in a patient with a history of alcohol abuse. There is no single laboratory marker that can definitively establish the diagnosis, but a number of biochemical derangements can be seen in these patients. The classical finding is an elevated aspartate aminotransferase (AST) level, two to six times the upper limit of normal, and an elevated alanine aminotransferase (ALT) level, to a lesser extent, resulting in an AST:ALT ratio of more than two. Leukocytosis, hyperbilirubinemia, and prolonged prothrombin time are also common.
Several scoring models have been developed to assess the severity of alcoholic hepatitis, predict mortality, and guide treatment decisions. The Maddrey discriminant function (DF) is widely used in the initial assessment of patients, with a value of 32 or higher signifying severe disease. The Lille score, which assesses the response of patients with severe alcoholic hepatitis to corticosteroid therapy, is another important scoring model. A Lille score of 0.45 or higher is associated with a 75% mortality rate at six months, indicating the need to discontinue corticosteroids.
Abstinence from alcohol use is the cornerstone of management in patients with alcoholic hepatitis. Complete sobriety is vital for the recovery of liver injury. However, studies have reported high rates of recidivism at six and 12 months in patients with severe alcoholic hepatitis. A recent study showed that the survival benefit of sobriety in alcoholic hepatitis was not apparent until 18 months following discharge, highlighting the need for immediate and sustained abstinence.
Chemo and Alcohol: Is Drinking Beer Safe?
You may want to see also