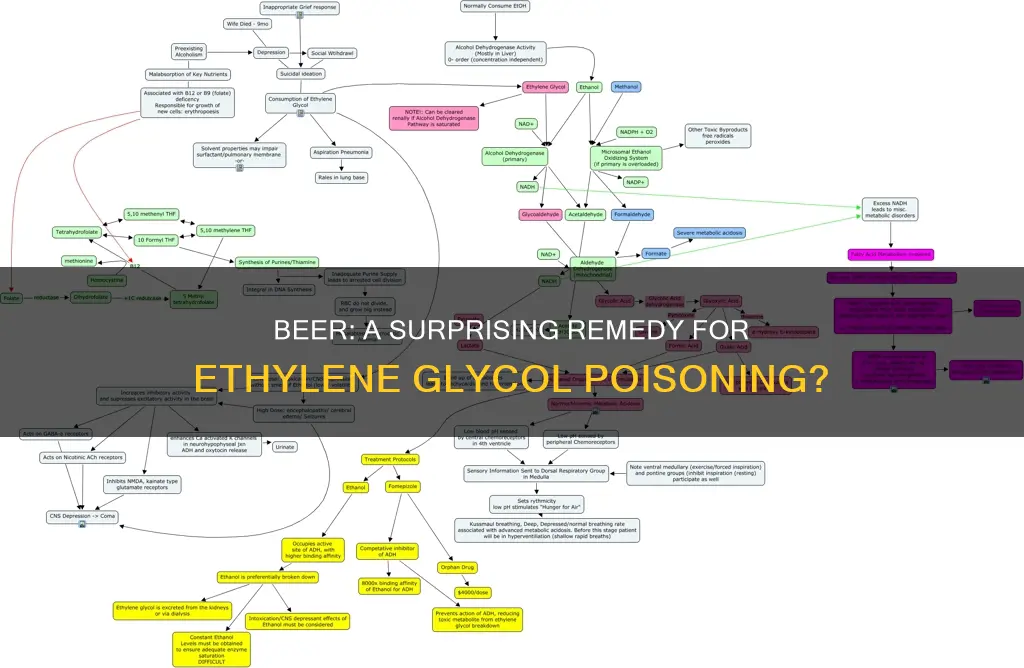
Ethylene glycol, a toxic alcohol commonly found in antifreeze, poses a serious health risk to humans and animals alike. Ingesting ethylene glycol can lead to severe health complications, including metabolic acidosis, kidney damage, and even death. The treatment for ethylene glycol poisoning typically involves the use of antidotes such as fomepizole or ethanol, which inhibit the formation of toxic metabolites. Interestingly, ethanol, in the form of alcoholic drinks like vodka, has been used as an antidote for ethylene glycol poisoning. This raises the question: can drinking beer reverse ethylene glycol poisoning? Beer, being an alcoholic beverage, contains ethanol, which acts as a competitive inhibitor of alcohol dehydrogenase, the enzyme responsible for metabolizing ethylene glycol. However, the effectiveness of beer in treating ethylene glycol poisoning is uncertain and requires further exploration.
| Characteristics | Values |
|---|---|
| Beer as an antidote for ethylene glycol poisoning | Beer (oral ethanol) can be used as an antidote for ethylene glycol poisoning. However, it is not the preferred treatment option. The preferred antidote is fomepizole, with ethanol (oral or intravenous) used if fomepizole is unavailable. |
| Effectiveness of beer as an antidote | Oral ethanol is effective in treating ethylene glycol poisoning, but it has limitations and side effects. It can be challenging to titrate and monitor, and it causes inebriation, requiring intensive care monitoring. Additionally, it is harder to dose accurately and requires close monitoring of serum ethanol concentration. |
| Advantages of beer over other antidotes | Beer (oral ethanol) is readily available in most hospitals, inexpensive, and can be administered orally or intravenously. |
| Disadvantages of beer compared to other antidotes | Beer (oral ethanol) has adverse effects, including intoxication, hypoglycemia in children, and possible liver toxicity. It also requires frequent blood ethanol concentration measurements and dosage adjustments. |
What You'll Learn

Beer as an antidote
Beer, or ethanol, can be used as an antidote for ethylene glycol poisoning. Ethylene glycol is a toxic alcohol commonly found in antifreeze, and its ingestion can be extremely dangerous and even life-threatening. The toxicity of ethylene glycol is due to its metabolites, glycolic acid and oxalic acid, which can cause metabolic acidosis and organ damage, particularly to the kidneys. The treatment for ethylene glycol poisoning involves stabilising the patient and administering an antidote to prevent the formation of these toxic metabolites.
Beer, or ethanol, acts as a competitive inhibitor of the enzyme alcohol dehydrogenase, which is responsible for the metabolism of ethylene glycol. By blocking the breakdown of ethylene glycol, beer helps to prevent the formation of its toxic metabolites and the associated nephrotoxic effects. This is particularly important as the toxicity and lethality of ethylene glycol are mainly due to its metabolites rather than the compound itself.
The use of beer as an antidote for ethylene glycol poisoning has been demonstrated in several case reports. In one case, a 42-year-old male car mechanic who accidentally ingested brake fluid was successfully treated with oral ethanol in the form of whisky through a nasogastric tube. Similarly, in a case report from India, a 70-year-old female who accidentally ingested ethylene glycol was treated with oral ethanol therapy through a nasogastric tube, along with hemodialysis. Both patients fully recovered without any complications.
The advantages of using beer or ethanol as an antidote include its wide availability in most hospitals and its low cost compared to other treatments. However, there are also some disadvantages to using beer or ethanol. It can be challenging to titrate and monitor the appropriate dosage, and it can cause intoxication, requiring intensive care monitoring. Additionally, ethanol therapy may result in adverse effects such as hypoglycaemia and liver toxicity.
It is important to note that while beer or ethanol can be used as an antidote for ethylene glycol poisoning, it is not the preferred treatment option. The current preferred treatment is fomepizole, a potent inhibitor of alcohol dehydrogenase. Fomepizole has been shown to be highly effective and is the only antidote approved by the US Food and Drug Administration for ethylene glycol poisoning. It is easier to dose, does not cause inebriation, and has minimal side effects. However, fomepizole is more expensive than ethanol, which may limit its accessibility in some settings.
In conclusion, beer or ethanol can be used as an effective antidote for ethylene glycol poisoning by inhibiting the formation of toxic metabolites. While it may not be the first-line treatment, it remains a valuable option, especially in resource-limited settings or when fomepizole is not readily available. However, it is important to carefully monitor patients receiving ethanol therapy and manage any associated side effects.
BYOB: Beer Gardens and Personal Alcohol Consumption
You may want to see also

Symptoms of ethylene glycol poisoning
Ethylene glycol poisoning can have serious health consequences, and even lead to death. The symptoms of ethylene glycol poisoning can be divided into three stages, with the first stage occurring within 30 minutes to 12 hours after ingestion. During this initial stage, individuals may experience neurological and gastrointestinal symptoms similar to alcohol poisoning. They may appear intoxicated, with slurred speech, seizures, dizziness, and lack of coordination. Stomach irritation, nausea, and vomiting are also common, along with excessive thirst and urination.
The second stage of ethylene glycol poisoning occurs between 12 and 36 hours after ingestion. While the signs of alcohol poisoning may appear to resolve, severe internal damage is still occurring. Symptoms during this stage include an elevated heart rate, hyperventilation, dehydration, high blood pressure, and metabolic acidosis. Low calcium concentrations in the blood, overactive muscle reflexes, muscle spasms, and congestive heart failure may also occur. This is the stage during which death is most likely to occur if left untreated.
The third and final stage of ethylene glycol poisoning occurs between 24 and 72 hours after ingestion and is characterised by kidney failure. Symptoms during this stage include severe lethargy, coma, depression, vomiting, seizures, and drooling. Other indicators of kidney failure include acute tubular necrosis, red blood cells in the urine, excess proteins in the urine, lower back pain, and decreased or absent urine production. If kidney failure occurs, it is typically reversible, but weeks or months of supportive care, including hemodialysis, may be required for kidney function to return.
It is important to note that poisoned individuals may not always develop each stage of symptoms, and the progression can vary. However, early treatment increases the chances of a good outcome. If you suspect ethylene glycol poisoning, seek medical help immediately.
Jehovah's Witnesses and Alcohol: Beer Included?
You may want to see also

Treatment options
Stabilisation and Decontamination
The most important initial treatment for ethylene glycol poisoning is stabilisation of the person. As ethylene glycol is rapidly absorbed, gastric decontamination is only likely to be beneficial if it is performed within 60 minutes of ingestion. The most common methods employed in ethylene glycol poisoning are gastric lavage or nasogastric aspiration of gastric contents. Ipecac-induced vomiting is not recommended. Activated charcoal does not adsorb glycols and is therefore not recommended.
Antidotes
The two antidotes for ethylene glycol poisoning are ethanol and fomepizole. These act by inhibiting alcohol dehydrogenase to stop the conversion of ethylene glycol into its toxic metabolites. When alcohol dehydrogenase is inhibited, the elimination half-life of ethylene glycol is prolonged from 4 to 6 hours to around 17 hours.
Ethanol can be given intravenously or orally, but its use should be limited to when fomepizole is inaccessible. It is less expensive than fomepizole but is harder to dose accurately, and requires close monitoring of the serum ethanol concentration. Ethanol may cause inebriation, which may necessitate intensive care monitoring.
Fomepizole is a more potent inhibitor of alcohol dehydrogenase than ethanol, and has been shown to be highly effective as an antidote for ethylene glycol poisoning. It is the only antidote approved by the U.S. Food and Drug Administration for the treatment of ethylene glycol poisoning. Fomepizole is more easily dosed, does not cause inebriation, and more strongly inhibits alcohol dehydrogenase, but is fairly expensive.
Haemodialysis
Haemodialysis is used to enhance the removal of unmetabolised ethylene glycol and its metabolites from the body. It is usually indicated in people with severe metabolic acidosis, kidney failure, severe electrolyte imbalance, or if the person's condition is deteriorating despite treatment. It is particularly important in the presence of renal dysfunction, severe metabolic acidosis, and severe electrolyte abnormalities.
Other Treatments
- Sodium bicarbonate may be helpful, particularly in severe metabolic acidosis, but is not universally considered a standard recommendation.
- Calcium gluconate may be indicated if complications occur due to hypocalcaemia, but should otherwise be replaced cautiously and judiciously, as exogenous calcium administration may enhance the precipitation of calcium oxalate crystals.
- Seizures in the presence of hypocalcaemia should be treated with benzodiazepines.
- Thiamine, pyridoxine, and magnesium may assist in shunting glycolic acid metabolism away from oxalic acid and toward its non-toxic metabolites.
RV Drinking Laws: Beer and Driving
You may want to see also

Diagnosis
Ethylene glycol poisoning is often difficult to diagnose as many of the clinical signs and symptoms are non-specific and similar to those of alcohol poisoning. Diagnosis is further complicated by the fact that many hospitals do not have the ability to perform tests to measure ethylene glycol levels in the blood. Therefore, diagnosis must often be based on the patient's presentation and a high index of suspicion.
The diagnosis of ethylene glycol poisoning should be considered in any person with a severe acidosis. The presence of calcium oxalate crystals in the urine or an increased osmol gap in the blood may also indicate ethylene glycol poisoning. Urine microscopy can reveal needle or envelope-shaped calcium oxalate crystals, which can suggest poisoning. However, these crystals may not be present until the late stages of poisoning.
In addition, many commercial radiator antifreeze products contain fluorescein, which can be detected using a Wood's lamp. Following ingestion of antifreeze products containing ethylene glycol and fluorescein, a Wood's lamp may reveal fluorescence in the person's mouth area, clothing, vomit, or urine, which can aid in diagnosing poisoning.
The most reliable method for diagnosing ethylene glycol poisoning is by measuring the blood ethylene glycol concentration using gas chromatography. However, this test is not readily available in all healthcare facilities. In such cases, diagnosis must be based on the patient's symptoms and the results of other laboratory tests.
When ethylene glycol poisoning is suspected, it is important to obtain a detailed history, including the time of ingestion, the amount ingested, and any co-ingestion of ethanol. A physical examination should be performed, including vital signs, neurological and cardiovascular assessments, and abdominal examination. Laboratory tests such as blood gas analysis, complete blood count, liver function tests, renal function tests, and electrolyte measurements are also important for diagnosis and monitoring.
It is crucial to act quickly when ethylene glycol poisoning is suspected, as early treatment increases the chances of a good outcome. Treatment should focus on stabilizing the patient, followed by the use of antidotes such as fomepizole or ethanol to inhibit the metabolism of ethylene glycol and prevent the formation of toxic metabolites.
Hot Beer: Is It Safe to Drink?
You may want to see also

Prevention
Ethylene glycol is a colourless, odourless, sweet-tasting liquid commonly found in antifreeze. It is extremely dangerous and can be life-threatening if left untreated. The toxicity and lethal dose of ethylene glycol is low, and even a small amount can be toxic and lead to death. Therefore, it is important to take preventive measures to avoid accidental or intentional ingestion, especially for young children and pets. Here are some preventive measures to avoid ethylene glycol poisoning:
- Keep ethylene glycol products in their original sealed containers and store them in places that are inaccessible to children and pets.
- Clean up any spills immediately and thoroughly. Use absorbent materials such as cat litter or sand to soak up the spill, and then dispose of it in a sealed plastic bag.
- Regularly check vehicles for leaks and address any issues promptly.
- If using antifreeze in toilets to prevent freezing, ensure the lid is closed and the bathroom door is kept closed.
- Dispose of used antifreeze responsibly by taking it to a service station or other designated disposal facility.
- Be cautious when using products containing ethylene glycol, such as windshield de-icing agents, brake fluid, motor oil, developing solutions for photography, wood stains, solvents, and paints.
- In aircraft de-icing and anti-icing operations, ensure proper handling and disposal of ethylene glycol to minimise its release into the environment.
- Be aware of the signs and symptoms of ethylene glycol poisoning, which can be similar to alcohol poisoning. Early symptoms include intoxication, vomiting, abdominal pain, dizziness, lack of coordination, drooling, and slurred speech.
- Seek immediate medical attention if ethylene glycol poisoning is suspected. Early treatment increases the chances of a good outcome.
Beer and Wine: Tips for Drinking Without Getting Sick
You may want to see also
Frequently asked questions
Ethylene glycol is a colourless, odourless, sweet-tasting liquid commonly found in antifreeze. It is toxic and dangerous to humans and animals.
Early symptoms include intoxication, vomiting, abdominal pain, incoordination, excessive thirst and urination. Later symptoms include decreased consciousness, headaches, seizures, kidney failure and brain damage.
Beer is not a recommended treatment for ethylene glycol poisoning. The preferred antidote is fomepizole, with ethanol (oral or intravenous) used if fomepizole is not available.