Drinking alcohol during chemotherapy is generally not recommended, as it can cause liver inflammation and interfere with the effectiveness of chemotherapy drugs. Alcohol can also worsen side effects such as dehydration, nausea, mouth sores, and vomiting. It is important to note that both chemotherapy and alcohol consumption may stress the kidneys, and alcohol may worsen chemotherapy-induced nausea. However, having an occasional beer or glass of wine during chemotherapy is unlikely to have serious effects, but it is always best to consult with a doctor.
| Characteristics | Values |
|---|---|
| Effect on platelet count | No evidence found |
| Safety | Depends on treatment regimen and liver function |
| Side effects | Dehydration, mouth sores, nausea, vomiting, sleep disturbances, depression, bone marrow suppression |
| Drug interactions | Matulane, Gleostine, Ultram, Anxiolytics, Antiemetics |
| Cancer risk | Alcohol is a known carcinogen |
What You'll Learn
- Beer and chemotherapy drugs are both processed by the liver
- Alcohol can cause liver inflammation which can interfere with chemotherapy
- Alcohol can worsen chemotherapy side effects like dehydration, diarrhoea, and mouth sores
- Alcohol can interfere with the production of blood cells
- Alcohol can increase the risk of certain cancers

Beer and chemotherapy drugs are both processed by the liver
It is not advisable to drink beer while on chemotherapy, as this could place additional stress on your liver. Both beer and chemotherapy drugs are processed by the liver, and drinking alcohol during chemotherapy can cause liver inflammation. This inflammation could impair the breakdown of chemotherapy drugs, thereby reducing their effectiveness.
The liver is responsible for breaking down and removing harmful substances from the body. When a person drinks alcohol, the liver metabolizes ethanol, converting it into acetaldehyde, which is toxic and can cause inflammation. Chemotherapy drugs are also metabolized by the liver, and this process can be disrupted if the liver is inflamed. This could lead to an increased risk of side effects from the chemotherapy treatment.
The liver is an important organ for detoxification and metabolism, and it plays a crucial role in maintaining the body's homeostasis. By drinking alcohol while on chemotherapy, individuals may be putting additional strain on their livers, potentially impairing their ability to process and eliminate the chemotherapy drugs effectively.
Additionally, alcohol consumption can worsen some of the side effects of chemotherapy, such as dehydration, diarrhoea, and mouth sores. It is important to note that excessive alcohol consumption is also associated with an increased risk of developing certain types of cancers.
Therefore, it is generally recommended that individuals undergoing chemotherapy avoid drinking alcohol, including beer, to ensure the optimal effectiveness of their treatment and to minimize the potential for adverse side effects. Consulting with a healthcare professional is always advised to determine the best course of action for an individual's specific situation.
Beer and Running: Is It Safe to Run After Drinking?
You may want to see also

Alcohol can cause liver inflammation which can interfere with chemotherapy
Drinking beer while undergoing chemotherapy is generally not recommended, as alcohol can interfere with the effectiveness of chemotherapy drugs. While an occasional beer or glass of wine is unlikely to cause serious harm, it is important to consult with your doctor before consuming any alcohol during chemotherapy.
Alcohol and chemotherapy drugs are both processed by the liver. Drinking alcohol during chemotherapy can cause liver inflammation, which can interfere with the chemotherapy's ability to do its job. This inflammation can reduce the liver's ability to break down and eliminate chemotherapy drugs from the body, leading to potential side effects or interactions.
In addition to liver inflammation, alcohol can also worsen certain side effects of chemotherapy, including dehydration, mouth sores, nausea, and vomiting. Alcohol can irritate the stomach and aggravate chemotherapy-induced nausea. It can also interfere with sleep and increase the risk of depression.
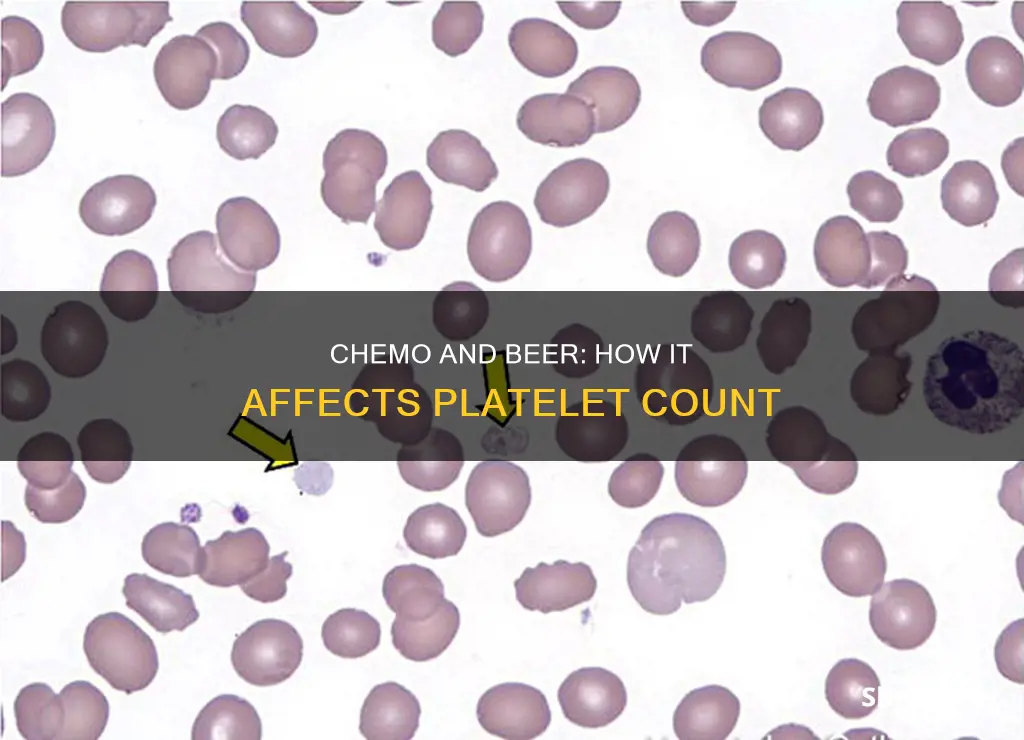
Furthermore, alcohol may interfere with the production of blood cells, potentially worsening bone marrow suppression in people undergoing chemotherapy. This can lead to a decrease in platelet count and other blood cells, which are crucial for fighting infections and supporting overall health during cancer treatment.
It is important to note that not all chemotherapy medications interact with alcohol in the same way. Some specific chemotherapy drugs, such as Matulane (procarbazine) and Gleostine (lomustine), are known to have severe side effects when combined with alcohol. Therefore, it is crucial to discuss your specific chemotherapy regimen with your healthcare team and follow their recommendations regarding alcohol consumption.
Beer and Atkins: What You Need to Know
You may want to see also

Alcohol can worsen chemotherapy side effects like dehydration, diarrhoea, and mouth sores
It is not advisable to drink alcohol while on chemotherapy. While an occasional beer or glass of wine is unlikely to have serious effects, it is always best to check with your doctor first. This is because some chemotherapy drugs can interact with alcohol and cause side effects such as dizziness, drowsiness, nausea, and vomiting.
Alcohol can also worsen chemotherapy side effects like dehydration, diarrhoea, and mouth sores. Both chemotherapy and alcohol consumption may stress the kidneys, and alcohol may cause dehydration, which may worsen nausea and make it difficult to tolerate necessary chemotherapy treatments. Alcohol is also known to irritate the stomach and aggravate the symptoms of chemotherapy-induced nausea.
Chemotherapy-induced mouth sores are common, and alcohol can make these sores worse and increase the pain. Alcohol can also cause liver inflammation, which can interfere with the effectiveness of chemotherapy drugs. This is because chemotherapy drugs and alcohol are both processed by the liver.
It is important to note that alcohol can also interfere with sleep and increase the risk of depression. Additionally, alcohol is a known cancer-causing agent, so it is generally recommended to avoid it during cancer treatment and limit consumption for overall survivorship.
Drinking Beer in an Uber: Is it Allowed?
You may want to see also

Alcohol can interfere with the production of blood cells
In addition, alcohol can cause structural abnormalities in blood cells, including platelets, leading to their premature destruction. This can result in a decrease in the number of functional platelets in the body. Alcohol can also interfere with the production and function of white blood cells, which are crucial for defending the body against bacteria and other foreign invaders. As a result, people who consume excessive amounts of alcohol may be more susceptible to infections.
Moreover, alcohol can affect the production and function of red blood cells, which are responsible for transporting oxygen and carbon dioxide throughout the body. Alcohol can cause a decrease in the number and function of red blood cells, leading to a condition called anemia. Anemia can cause fatigue, shortness of breath, lightheadedness, and other health issues.
Overall, alcohol's interference with the production and function of blood cells, including platelets, can have significant negative consequences for overall health and increase the risk of various medical complications.
Beer and Chemo: What's Safe?
You may want to see also

Alcohol can increase the risk of certain cancers
Drinking beer while on chemotherapy is generally not recommended. While having an occasional beer or glass of wine during chemotherapy is unlikely to have serious effects, it's important to consult your doctor or healthcare team first. Some chemotherapy drugs can interact with alcohol and could make you unwell.
Now, onto the topic of alcohol and its link to cancer. Alcohol can indeed increase the risk of certain cancers. According to the National Institutes of Health (NIH), about 5.5% of all new cancer diagnoses and 5.8% of all cancer-related deaths are attributed to drinking alcohol. The more alcohol a person consumes, especially over time, the higher their risk of developing an alcohol-associated cancer. Even those who have no more than one drink per day and binge drinkers have a slightly increased risk of certain cancers.
- Acetaldehyde production: When the body breaks down ethanol (the type of alcohol in alcoholic drinks), it produces acetaldehyde, a known carcinogen that damages DNA and impairs cells' ability to repair that damage, allowing cancerous cells to grow.
- Hormonal effects: Alcohol can affect hormone levels, such as estrogen, which can increase the risk of certain cancers, including estrogen-receptor-positive breast cancer.
- Reduced nutrient absorption: Alcohol interferes with the absorption of vital nutrients that protect the body from cancer, including vitamins A, B1, B6, C, D, E, K, and folate, as well as minerals like iron and selenium.
- Weight gain: Alcohol contributes to excess calorie intake, and obesity is a risk factor for over 12 types of cancer.
- Tobacco-related cancers: Alcohol use, when combined with tobacco use, significantly increases the risk of oral, throat, and other cancers.
The types of cancer linked to alcohol consumption include:
- Head and neck cancers: Moderate to heavy drinking is associated with higher risks.
- Esophageal cancer: Any level of alcohol consumption increases the risk of esophageal squamous cell carcinoma.
- Liver cancer: Heavy alcohol consumption is associated with a nearly doubled risk of certain types of liver cancer.
- Breast cancer: The risk increases with alcohol intake, with light drinkers having a slightly increased risk and heavy drinkers a much higher risk.
- Colorectal cancer: Moderate to heavy alcohol consumption increases the risk of cancers of the colon and rectum.
- Stomach and pancreatic cancers: Studies show that drinking three or more alcoholic drinks per day increases the risk of these cancers.
- Prostate cancer: There is evidence that alcohol consumption is associated with an increased risk, although the link is not yet fully understood.
It's important to note that the risk of developing these cancers varies based on the amount and frequency of alcohol consumption. The recommended guidelines for alcohol consumption, according to the Dietary Guidelines for Americans, suggest that men should have no more than two drinks per day, and women should have no more than one drink per day. However, the best way to reduce the risk of alcohol-related cancers is to abstain from drinking alcohol altogether.
Beer and Weight Loss: Is It Possible to Have Both?
You may want to see also
Frequently asked questions
It is not recommended to drink alcohol while on chemotherapy. Alcohol can cause liver inflammation, which can interfere with the effectiveness of chemotherapy drugs. Alcohol may also worsen side effects such as dehydration, nausea, and mouth sores. It is best to consult with your doctor about whether it is safe to consume alcohol during your treatment.
Alcohol can interfere with the production of blood cells, potentially worsening bone marrow suppression in people undergoing chemotherapy. This can lead to a decrease in platelet count.
In addition to interfering with the production of blood cells and worsening side effects, alcohol can also decrease your immune system and cause liver inflammation. Alcohol is also a known carcinogen, increasing the risk of developing certain types of cancer. It is important to discuss any alcohol consumption with your healthcare team during chemotherapy.







