Hepatitis C is a viral infection of the liver, and alcohol is a known liver toxin. The first instruction typically given to anyone diagnosed with Hepatitis C is to abstain from drinking alcohol. While heavy drinking is linked to more severe liver problems, there is no safe level of drinking for people with this virus. Alcohol can exacerbate HCV infection and the associated liver damage by causing oxidative stress and promoting fibrosis, accelerating the disease's progression to cirrhosis. It can also make HCV treatments ineffective and impair the body's immune defence against the virus. Even after eliminating the virus from the body, alcohol still poses a threat to the liver's health. Therefore, it is recommended to talk to a medical provider about alcohol consumption after curing Hepatitis C, as there is no clear data or medical consensus.
| Characteristics | Values |
|---|---|
| Can I drink beer after being cured of Hep C? | There is no clear medical consensus on this issue. Some doctors recommend total abstinence from alcohol, while others are fine with an occasional standard-sized drink. |
| Why is there no clear consensus? | There is a lack of clear data and comprehensive studies on the effect of alcohol consumption after being cured of Hep C. |
| What are the risks of drinking alcohol after being cured of Hep C? | Alcohol is a known liver toxin and can cause liver damage, including inflammation, scarring, and fat buildup. It can also negatively affect the effectiveness of Hep C treatments and increase the risk of liver disease and liver cancer. |
| What are the recommendations for people with liver disease? | For people with advanced liver disease, such as cirrhosis, or other liver diseases such as fatty liver disease, it is recommended to avoid alcohol completely. |
| What is considered moderate drinking? | Light drinking is typically defined as no more than two drinks per week, while moderate drinking is defined as no more than 14 drinks per week. |
What You'll Learn
- Alcohol is a known liver toxin and can cause inflammation, scarring and fat build-up
- There is no safe level of drinking for people with the Hepatitis C virus
- Doctors recommend not drinking alcohol while being treated for Hepatitis C as it negatively affects the way medicines work
- Alcohol dependence can be a challenge for those with Hepatitis C, and relapse is a risk
- Even after curing Hepatitis C, alcohol still poses a threat to the liver

Alcohol is a known liver toxin and can cause inflammation, scarring and fat build-up
Alcohol is a well-known toxin to the liver and can cause inflammation, scarring, and fat build-up. This is due to the chemical reaction that occurs when the liver breaks down alcohol, which releases toxins that damage liver cells. Alcohol-associated liver disease (ALD) is the result of drinking more alcohol than the liver can process, which damages the organ.
There are three types of ALD: steatotic (fatty) liver, acute hepatitis, and cirrhosis. Steatotic liver is the most common alcohol-induced liver problem and is caused by fat accumulating inside liver cells, making it hard for the liver to function properly. Acute hepatitis is an acute inflammation of the liver that results in liver cell death and permanent scarring. Cirrhosis is the most serious form of ALD and occurs when the entire liver is scarred, causing the organ to shrink and harden, which can lead to liver failure.
Alcohol-associated liver disease is caused by heavy alcohol use and is both preventable and potentially fatal. The liver's job is to break down alcohol, but if you drink more than it can process, it can become badly damaged. Heavy alcohol use is defined as consuming more than 14 grams of pure alcohol (ethanol) per day or more than 14 drinks per week for men, and consuming more than 11 grams of pure alcohol (ethanol) per day or more than 7 drinks per week for women.
If you have been cured of hepatitis C, the recommendation regarding alcohol consumption is controversial. Some patients feel strongly about abstaining from alcohol, while others may feel comfortable with an occasional drink. If you have advanced liver disease, such as cirrhosis, or another liver disease such as fatty liver disease, it is recommended to avoid alcohol completely. For those with minimal liver disease and no history of alcohol problems, there is no clear data or medical consensus. It is important to consult with a healthcare provider to determine what is safe for your individual situation.
Beer and Cefdinir: Is It Safe to Mix?
You may want to see also

There is no safe level of drinking for people with the Hepatitis C virus
Drinking alcohol after curing hepatitis C is a controversial issue. While some patients feel strongly about abstaining from alcohol, others would like an occasional drink, especially during special events. However, it is important to note that there is no safe level of alcohol consumption for people who have had hepatitis C.
Hepatitis C is a liver disease caused by the hepatitis C virus (HCV). The virus causes inflammation, which can affect overall liver function and lead to liver damage, scarring, and cancer. Alcohol consumption can also cause inflammation in the liver and create scar tissue. Therefore, drinking alcohol can increase the damage caused by HCV and negatively impact treatment effectiveness.
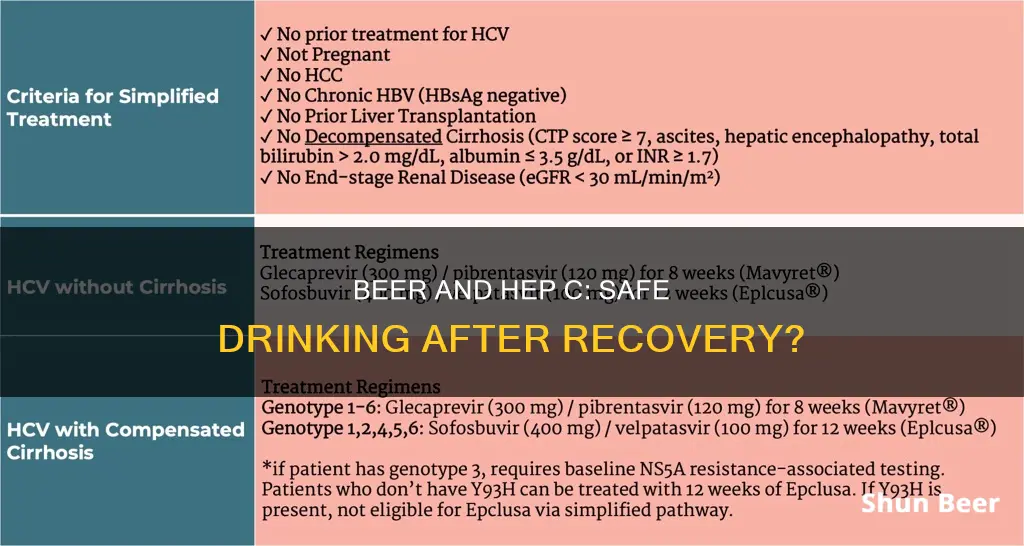
If you have advanced liver disease, such as cirrhosis, or another liver disease, such as fatty liver disease, it is recommended to avoid alcohol completely. Alcohol can also interfere with the effectiveness of HCV treatments, including oral antiviral medications and interferon. Even after achieving a sustained virologic response (SVR) and curing HCV, doctors generally recommend refraining from drinking alcohol.
It is crucial to have open and honest conversations with your doctor about alcohol consumption and HCV. Your doctor can help you create the best care plan for your needs and ensure the effectiveness of your treatment. While there may not be clear data or a medical consensus on alcohol consumption for those cured of HCV, avoiding alcohol is always the safest option for liver health.
Beer after wine: Is it a good idea?
You may want to see also

Doctors recommend not drinking alcohol while being treated for Hepatitis C as it negatively affects the way medicines work
Doctors recommend that you refrain from drinking alcohol while being treated for Hepatitis C. This is because alcohol negatively affects the way Hepatitis C medicines work in your body.
Hepatitis C is a viral infection of the liver, and alcohol is a known liver toxin. The liver breaks down most of the alcohol you consume so that it can be removed from the body. To break down the alcohol, the liver creates proteins that speed up chemical reactions in the body (enzymes). During this process, the enzymes can also create scar tissue and cause your liver to build up fat. Alcohol also causes inflammation in the liver.
Hepatitis C can damage the liver, and this damage is increased if you consume alcohol. Alcohol can also make Hepatitis C treatments ineffective. While there is not a lot of information about how alcohol affects oral antiviral medicines, people in Hepatitis C drug trials were not allowed to drink alcohol. Because of this, doctors do not know if alcohol causes these medicines to be less effective. However, doctors do know that alcohol makes the injectable drug interferon, which is sometimes used to treat Hepatitis C, less effective.
Even after successfully eliminating the Hepatitis C virus, the reasons for abstaining from alcohol remain valid. The viral particles may no longer be present, but alcohol still poses a threat to the liver's health. During the course of the infection, damage to the liver could range from minimal to severe. Those who escaped with little liver damage have a better prognosis than those who lost functioning liver cells.
If you have achieved a sustained virologic response (SVR) and have no detectable liver injury from the virus, then one glass of wine per month is probably okay. However, for anyone else who achieved SVR, putting alcohol back into the picture is risky.
Exploring Beer Drinking Rules in National Parks
You may want to see also

Alcohol dependence can be a challenge for those with Hepatitis C, and relapse is a risk
The prevalence of HCV infection is higher among patients with AUD who are current or past injecting drug users. Within a cohort of patients with AUD admitted for hospital detoxification in Barcelona, Spain, HCV prevalence was as high as 20%. HCV infection is also more prevalent among people with alcohol abuse disorder, even in those without other HCV risk factors.
Alcohol abuse and HCV infection are associated with increased morbidity and mortality. HCV antiviral therapy is less commonly prescribed in individuals with both conditions. Alcohol consumption is associated with more extensive liver damage in HCV-infected patients, and there is no safe level of alcohol consumption for those with the virus. Even moderate alcohol consumption by HCV-infected patients can lead to progressive liver fibrosis.
Alcohol consumption can also interfere with HCV treatment. Heavy drinking during antiviral (interferon) treatment has been shown to impede patients' responses to therapy. Abstaining from drinking before and during treatment improves patients' response to antiviral therapy, although this improvement is not total.
In light of these findings, alcoholic patients should be advised to abstain from further alcohol consumption and should be alcohol-free for at least 6 months before beginning interferon therapy.
Drinking Beer in the Back Seat: What's the Law?
You may want to see also

Even after curing Hepatitis C, alcohol still poses a threat to the liver
Hepatitis C is a viral infection of the liver that can lead to severe complications, including permanent scarring of the liver (cirrhosis), liver damage, liver scarring, and liver cancer. While curing Hepatitis C is a significant achievement, it is essential to understand that the threat to liver health doesn't disappear completely. Alcohol consumption, even in moderate amounts, can still pose a significant risk to liver health and function.
The liver is primarily responsible for filtering toxins and waste from the blood and body. When alcohol is consumed, the liver breaks it down and creates proteins that speed up chemical reactions in the body (enzymes). This process can lead to the creation of scar tissue and fat build-up in the liver, causing inflammation and potential long-term damage.
Even after successfully curing Hepatitis C, the liver may have sustained some level of damage, ranging from minimal to severe. Consuming alcohol can put the remaining healthy liver cells at risk and potentially trigger a relapse of liver damage. The severity of liver disease is a critical factor in determining the risks associated with alcohol consumption. For individuals with liver disease that has progressed beyond mild fibrosis, drinking alcohol can be particularly dangerous and may cause similar damage to that caused by the Hepatitis C virus.
Additionally, alcohol dependence or addiction can further complicate the decision to consume alcohol. For those who struggled with abstaining during their treatment, returning to alcohol consumption can easily trigger a relapse into excessive drinking, which is extremely dangerous for a liver that is recovering from Hepatitis C infection.
While there is a lack of comprehensive studies on the effect of alcohol consumption after curing Hepatitis C, the available evidence suggests that alcohol continues to pose a significant threat to liver health. The decision to consume alcohol should be made in consultation with a medical professional, who can assess the individual's liver health, degree of liver damage, and risk factors.
In conclusion, while curing Hepatitis C is a significant milestone, it is important to recognize that alcohol still poses a threat to the liver. The potential risks associated with alcohol consumption should be carefully considered, and individuals should work closely with their medical providers to make informed decisions regarding their health and well-being.
Beer and Klonopin: Safe Mix or Risky Business?
You may want to see also







