Alcohol negatively impacts the liver, and long-term alcohol abuse can lead to a condition called alcohol cirrhosis. Alcohol is mainly broken down in the liver, and heavy drinking can result in the destruction of normal liver tissue or death of liver cells, leaving behind scar tissue. This can lead to alcoholic hepatitis, an acute inflammation of the liver that can be fatal without treatment.
The liver's main actions include breaking down and filtering harmful substances in the blood, as well as manufacturing proteins, enzymes, and hormones. It also converts vitamins, nutrients, and medicines into substances that our bodies can use. The liver processes over 90% of the alcohol a person consumes, and the rest is eliminated from the body.
The amount of alcohol that causes cirrhosis varies. For cirrhosis to develop in men, a person must drink more than about 3 ounces of alcohol a day for more than 10 years. These 3 ounces include drinking 6 cans of beer, 5 glasses of wine, or 6 shots of liquor. Women may develop liver cirrhosis if they drink half the amount of alcohol as men, which means drinking more than 1.5 ounces of alcohol a day for several years.
Heavy drinkers or alcoholics face a higher risk of developing liver disease compared to moderate or non-drinkers. For instance, many heavy drinkers develop fatty liver disease, which is usually reversible with abstinence. Alcoholic hepatitis, or inflammation of the liver, may also occur and is reversible with abstinence. However, if treatment is not received in time, this condition can cause liver degeneration, which may progress to cirrhosis and can even be fatal.
| Characteristics | Values |
|---|---|
| Alcohol-induced liver disease types | Steatotic (fatty) liver, acute hepatitis, cirrhosis |
| Alcohol-induced liver disease causes | Heavy use of alcohol, long-term unhealthy alcohol use |
| Alcohol cirrhosis | Destruction of normal liver tissue or death of liver cells, leaving scar tissue in its place |
| Alcoholic hepatitis | Acute inflammation of the liver that can be fatal without treatment |
| Liver's main actions | Breaking down and filtering out harmful substances in the blood, manufacturing proteins, enzymes, and hormones, converting vitamins, nutrients, and medicines into substances the body can use, cleaning out blood, producing bile for digestion, storing glycogen for energy |
| Liver cirrhosis causes | Excessive drinking of alcohol, hepatitis B and C virus infections, fatty liver caused by obesity and diabetes |
| Alcoholic liver cirrhosis causes | Excessive and chronic alcohol consumption |
| Non-alcoholic fatty liver disease (NAFLD) causes | Obesity, high blood cholesterol and triglycerides |
What You'll Learn

Alcohol consumption and liver cirrhosis: a systematic review and meta-analysis
Alcohol consumption is a major risk factor for liver cirrhosis, with the risk increasing exponentially. While the liver is responsible for breaking down alcohol, excessive consumption can lead to serious damage, resulting in a condition called alcohol cirrhosis. This involves the destruction of normal liver tissue and cell death, leading to scarring and potentially fatal inflammation.
A systematic review and meta-analysis of the relationship between alcohol consumption and liver cirrhosis was conducted by Michael Roerecke and colleagues in 2019. The study analysed data from over 2.6 million participants, with 5,505 cases of liver cirrhosis. The results indicated that women may be at higher risk of liver cirrhosis than men, even with relatively low alcohol consumption. For example, consuming one drink per day increased the risk for women but not for men, compared to long-term abstainers. Drinking five or more drinks per day significantly increased the risk for both sexes, with a higher relative risk for women.
The study also highlighted the need for further high-quality research to understand the role of other risk factors, such as genetic factors, body weight, metabolic factors, and drinking patterns. It emphasised the importance of avoiding high alcohol consumption and recommended interventions to reduce intake for those drinking at high levels.
Beer and Blood Tests: Drinking Before a CBC
You may want to see also

The impact of drinking patterns on cirrhosis risk
Alcohol consumption is a major risk factor for liver cirrhosis, with risk increasing exponentially. The impact of drinking patterns on the risk of cirrhosis is complex and influenced by various factors, including the amount and frequency of alcohol consumption, drinking with or without meals, type of beverage, and individual characteristics such as genetic vulnerability, body weight, metabolic risk factors, and smoking status.
Amount and Frequency of Alcohol Consumption:
- The risk of cirrhosis increases with the total amount of alcohol consumed, even at moderate levels.
- Drinking seven or more drinks per week is associated with a higher risk of cirrhosis compared to consuming fewer drinks per week.
- Daily drinking is associated with a higher risk of cirrhosis compared to non-daily drinking, even when controlling for the total amount of alcohol consumed.
Drinking with or without Meals:
Drinking alcohol with meals is associated with a lower risk of cirrhosis compared to drinking without meals, even when adjusting for the amount of alcohol consumed.
Type of Beverage:
The type of alcohol consumed may also influence the risk of cirrhosis. Some studies suggest that drinking wine may be associated with a lower risk compared to drinking other types of alcohol, but the findings are inconsistent.
Individual Characteristics:
- Genetic vulnerability: Twin studies suggest a higher disease concordance among monozygotic twins compared to dizygotic twins, indicating a possible genetic link. However, genetic case-control studies have not yet provided conclusive results.
- Body weight and metabolic risk factors: Obese individuals may be more susceptible to the harmful effects of alcohol consumption on the liver.
- Smoking: Smoking is a confounding factor in the relationship between alcohol consumption and cirrhosis risk, with smokers having a higher risk than non-smokers.
Overall, the evidence suggests that drinking patterns have a significant impact on the risk of cirrhosis. Heavy and frequent alcohol consumption, especially when not accompanied by meals, increases the risk of cirrhosis. However, it is important to note that even moderate levels of alcohol consumption can increase the risk, and individual characteristics may also play a role in modifying this risk.
Beer and Xanax: A Risky Mix?
You may want to see also

Alcohol's effect on liver cells
Alcohol negatively impacts the liver and is the primary cause of alcohol-associated liver disease (ALD). The liver is responsible for breaking down alcohol, and if you drink more than it can process, it can become badly damaged. The liver has many functions, including:
- Filtering toxins from the blood
- Aiding digestion of food
- Regulating blood sugar and cholesterol levels
- Helping fight infection and disease
The liver is resilient and can regenerate itself, but prolonged alcohol misuse over many years can reduce its ability to regenerate, resulting in serious and permanent damage. ALD has several stages of severity and a range of associated symptoms. The first stage is alcoholic fatty liver disease, which rarely causes symptoms but is a warning sign that you're drinking at a harmful level. The second stage is alcoholic hepatitis, which is a potentially serious condition that can be caused by alcohol misuse over a longer period or by binge drinking. The third stage is cirrhosis, where the liver has become significantly scarred, and this is generally not reversible.
The liver processes over 90% of the alcohol a person consumes, and the rest is eliminated from the body. It usually takes the body about an hour to process one alcoholic drink, and this time frame increases with each drink. The higher the amount of alcohol in the system, the longer it takes for the body to process it. The liver can only process a certain amount of alcohol at one time, and the rest of the unprocessed alcohol that remains in the liver eventually makes its way into the bloodstream. This is the point at which people become intoxicated or drunk. Drinking like this on a daily basis can destroy liver cells, causing the liver to scar (a condition known as cirrhosis), alcoholic hepatitis, and cellular mutation that can result in cancer.
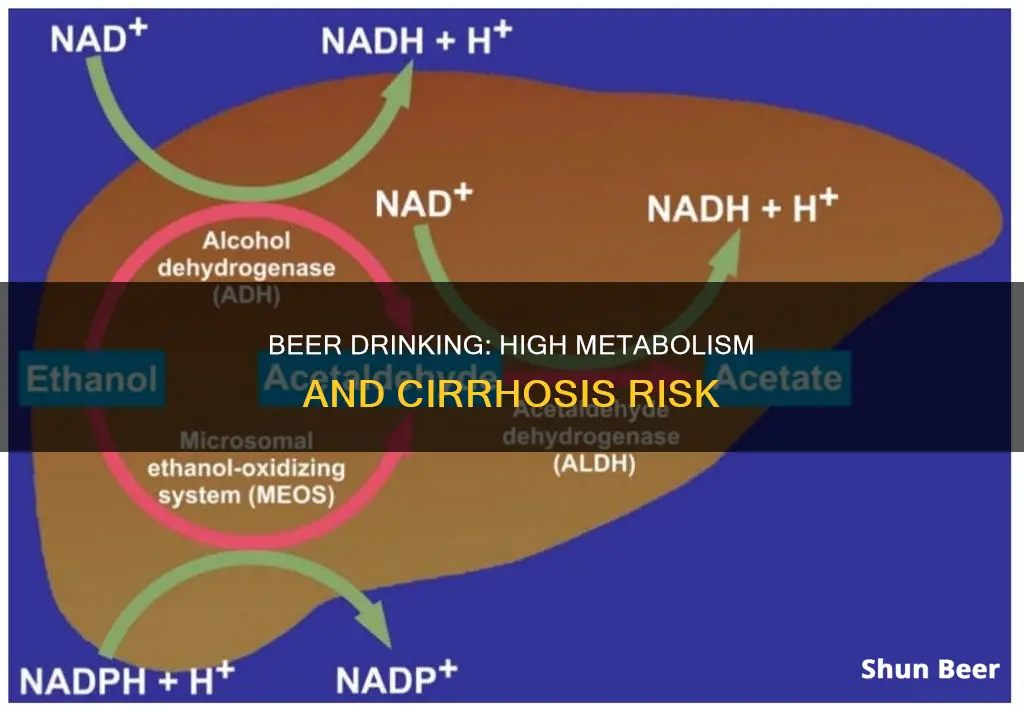
Alcohol is broken down in the liver by the enzyme alcohol dehydrogenase (ADH). This enzyme converts alcohol to acetaldehyde through a process called oxidation. Acetaldehyde is highly toxic to the body and is rapidly oxidised to acetate by the enzyme aldehyde dehydrogenase (ALDH). Most of the acetate then travels through the bloodstream to other parts of the body. The You may want to see also Alcohol-induced liver disease is caused by heavy alcohol use, which is defined as consuming more than the liver can process. The liver's job is to break down alcohol, and if you drink more than it can handle, it can become badly damaged. The effects of alcohol on the liver depend on how much and how long you've been drinking. There are three types of alcohol-induced liver disease: Non-alcoholic fatty liver disease (NAFLD), on the other hand, is very common, affecting about 1 in 3 adults in the US. It is not caused by alcohol consumption but is instead linked to obesity and diabetes. NAFLD does not usually cause symptoms, but it can progress to a more serious form called non-alcoholic steatohepatitis (NASH), which can lead to liver scarring, cancer, and eventually liver failure. While alcohol-induced liver disease and NAFLD have some similar symptoms, their causes and treatments differ. For alcohol-induced liver disease, the most important part of treatment is to stop drinking alcohol completely. Dietary changes may also be recommended. With complete alcohol avoidance and time, the liver can often heal some of the damage caused by alcohol. However, if the liver tissue loss is severe enough to cause liver failure, most of the damage may be permanent, and a liver transplant may be necessary. In contrast, NAFLD can be treated with weight loss, a healthy diet, and exercise. You may want to see also The liver is a vital organ that performs hundreds of functions essential for our health, including processing food, medicine, alcohol, and other toxins. Alcohol-related liver disease is common but preventable. It occurs after prolonged heavy drinking and is more prevalent among those who are physically dependent on alcohol. The liver's job is to break down alcohol, and excessive consumption can lead to serious damage. Gender Differences in Alcohol-Related Liver Disease Research shows that clear differences exist in liver health and disease between women and men. While men are more likely to experience alcoholic liver disease due to higher rates of alcohol use disorder, women with alcoholic liver disease exhibit more rapid progression to fibrosis and cirrhosis. This disparity is attributed to various biological and social factors. Biological Factors Women generally have lower body water content and produce smaller amounts of alcohol dehydrogenase, an enzyme that breaks down alcohol in the bloodstream. As a result, women's bodies are more susceptible to the damaging effects of alcohol, and a smaller amount of alcohol can lead to liver problems. Additionally, women tend to have higher blood ethanol levels after consuming the same amount of alcohol as men due to differences in gastric alcohol dehydrogenase activity and the first-pass metabolism of alcohol in the stomach. Social Factors The social stigma attached to drinking has declined, and alcohol is now more readily available in supermarkets. These factors have contributed to the increasing prevalence of alcoholism among women. However, men still have greater opportunities for drinking, as reflected in national surveys and consumption data. Autoimmune Liver Disorders Autoimmune liver disorders, such as primary biliary cholangitis and autoimmune hepatitis, are much more common in women than in men. While alcohol consumption may exacerbate these conditions, they are not caused by alcohol use. The exact reasons for this disparity are unknown, but sex hormones are believed to play a role, influencing gene expression and immune response receptors. Tumor Presentation Liver tumor presentation also differs between genders, with benign tumors more common in women and malignant tumors more prevalent in men. For example, hepatocellular adenoma, a rare benign tumor, primarily affects reproductive-age women and is associated with oral contraceptive use. On the other hand, hepatocellular carcinoma, the most common form of liver cancer, occurs more frequently in men. Drug-Induced Liver Injury Women are more susceptible to drug-induced liver injury and acute liver failure. In a study, women accounted for over 70% of patients hospitalized with acute liver injury due to acetaminophen and unintended drug reactions. This female preponderance may be related to sex-based differences in the expression of genes affecting liver metabolic function. A better understanding of gender differences in alcohol-related liver disease is crucial for improving health outcomes and providing individualized care. While some factors, such as biological differences in alcohol metabolism, contribute to the disparity, social factors, including changing societal norms and alcohol availability, also play a significant role. Further research is needed to elucidate the exact mechanisms behind these gender differences and develop effective strategies to address them. You may want to see also Yes, drinking beer can lead to cirrhosis, especially when consumed in large quantities over a long period. A high metabolism may not directly reduce the risk of cirrhosis from drinking beer. However, individuals with a higher metabolism may process alcohol faster, reducing the amount of time the liver is exposed to harmful substances. Symptoms of cirrhosis include spidery red veins on the skin, yellowing of the skin and eyes, reddened palms, fluid retention in the abdomen and legs, internal bleeding, hormone disruptions, disturbed sleep patterns, and cognitive problems. To prevent cirrhosis, it is important to avoid excessive alcohol consumption and maintain a healthy weight to reduce the risk of non-alcoholic fatty liver disease.Drinking Beer in Public: Las Vegas Laws and Where to Enjoy

Alcohol-induced liver disease vs non-alcoholic fatty liver disease
Wine, Beer, and Mixing Drinks: What's the Verdict?

The role of gender in alcohol-related liver disease
Drinking Beer Through a Straw: Is It Possible?
Frequently asked questions