Drinking alcohol, including beer, during chemotherapy is generally not recommended. While the occasional beer or glass of wine is unlikely to have serious effects, it's important to consult with your doctor first, as some chemotherapy drugs can interact with alcohol and cause adverse effects. Excessive alcohol consumption during chemotherapy can worsen side effects such as dehydration, diarrhoea, and mouth sores, and it can also place additional stress on the liver, which processes both alcohol and chemotherapy drugs. It's worth noting that drinking alcohol is associated with a higher risk of developing several types of cancer and can increase the risk of recurrence for cancer survivors. Therefore, limiting alcohol consumption or abstaining during chemotherapy is generally advisable.
| Characteristics | Values |
|---|---|
| Occasional beer after chemotherapy | Generally, having an occasional beer or glass of wine after chemotherapy is unlikely to have serious effects. |
| Frequent or heavy drinking after chemotherapy | Can worsen chemotherapy side effects, such as dehydration, diarrhea, and mouth sores. |
| Alcohol and chemotherapy drugs | Both are processed by the liver, so drinking while on chemotherapy can place additional stress on your liver. |
| Alcohol and cancer risk | Drinking alcohol is associated with a higher risk of developing several types of cancer. |
| Alcohol and cancer recurrence risk | Studies show that breast cancer survivors who drank more than three to four drinks per week were at a higher risk for recurrence. |
What You'll Learn

Occasional beer drinking is unlikely to affect chemotherapy
While undergoing chemotherapy, it is generally advised to avoid drinking alcohol. However, having an occasional beer or two during this time is unlikely to cause any serious harm or affect the treatment's effectiveness.
Chemotherapy drugs vary, and some may interact with alcohol, so it is crucial to consult your doctor or healthcare team before consuming any alcoholic beverages. They will advise you on whether it is safe to drink in moderation and ensure it will not interfere with your specific treatment plan.
It is important to remember that excessive alcohol consumption is never advisable, especially during cancer treatment. Alcohol can worsen certain side effects of chemotherapy, such as dehydration, diarrhoea, and mouth sores. Additionally, both alcohol and chemotherapy drugs are processed by the liver, so drinking while undergoing chemotherapy can place additional stress on this vital organ.
Furthermore, drinking alcohol has been linked to an increased risk of developing several types of cancer, and for cancer survivors, it may increase the chances of the cancer returning. Therefore, limiting alcohol consumption, or abstaining completely, is generally recommended to reduce long-term cancer risk.
If you choose to drink occasionally during chemotherapy, ensure you follow your doctor's recommendations and do not exceed safe limits.
Beer and MRI: What You Need to Know
You may want to see also

Check with your doctor before drinking beer
It's important to check with your doctor before drinking beer after chemotherapy. While an occasional beer or glass of wine during chemotherapy is unlikely to have serious effects, it's always good to be cautious. Some chemotherapy drugs can interact with alcohol and could make you unwell, so it's important to get medical advice first. Your doctor will know which medications you are taking and can advise if it is safe for you to consume alcohol.
Alcohol is processed by the liver, and so are many chemotherapy medications. Consuming alcohol while on chemotherapy can place additional stress on your liver, which is something to be avoided. Alcohol can also worsen some side effects of chemotherapy, such as dehydration, diarrhoea, and mouth sores. If you have mouth sores, alcohol may sting, particularly spirits. If you are feeling sick during chemotherapy, alcohol may make this worse.
Additionally, drinking alcohol has not been shown to reduce cancer risk. In fact, studies have found that alcohol consumption is associated with a higher risk of developing several types of cancer. For people being treated for cancer, drinking alcohol can also have other harmful consequences, such as making their treatments less effective. For cancer survivors, regular alcohol use may increase the chances of cancer returning.
If you choose to drink alcohol after chemotherapy, it is generally recommended to limit consumption to no more than one drink per day for women and two drinks per day for men. However, it's important to remember that these are general guidelines and may not apply to everyone. Always consult your doctor to get personalized advice based on your specific situation.
Beer and Milkshakes: Mixing Drinks, Safe or Not?
You may want to see also

Alcohol can worsen chemotherapy side effects
Liver Inflammation
Many chemotherapy drugs are broken down by the liver, and so is alcohol. Alcohol consumption can cause liver inflammation, which may impair the breakdown of chemotherapy drugs and increase their side effects.
Mouth Sores
Chemotherapy often causes mouth sores, and alcohol can irritate them or make them worse.
Nausea and Vomiting
Alcohol is known to irritate the stomach and can aggravate chemotherapy-induced nausea and vomiting. It can also worsen dehydration caused by vomiting, diarrhea, or excessive urination, which are common side effects of chemotherapy.
Blood Counts
Alcohol interferes with the production of blood cells and can worsen bone marrow suppression in people undergoing chemotherapy.
Peripheral Neuropathy
Chronic alcohol use can worsen chemotherapy-induced peripheral neuropathy, which causes painful tingling in the hands and feet.
Sleep Disturbances and Depression
Alcohol can disrupt sleep, and poor sleep corresponds to poorer survival times in people with advanced cancer. As a depressant, alcohol can also worsen depression and make it harder for people to cope during chemotherapy.
Beer and Bypass Surgery: What You Need to Know
You may want to see also

Alcohol may make chemotherapy less effective
Alcohol can also cause side effects when combined with certain chemotherapy drugs, such as Matulane (procarbazine) and Gleostine (lomustine). It can also interact with painkillers, anti-anxiety drugs, and anti-nausea medications used to support cancer treatment. For example, Ultram (tramadol), a painkiller, can cause excessive drowsiness and confusion when mixed with alcohol. Using alcohol with Ultram can also severely suppress breathing, blood pressure, and heart rate. Similarly, anti-anxiety drugs like Xanax (alprazolam) and Ativan (lorazepam) can cause extreme sleepiness, difficulty concentrating, and abnormally slowed breathing when mixed with alcohol. Alcohol can also cause extreme drowsiness, dizziness, and loss of coordination when combined with anti-nausea drugs like Zofran (ondansetron).
In addition, alcohol can worsen chemotherapy-related side effects. For example, the dehydrating effect of alcohol can worsen any dehydration caused by chemotherapy (typically due to vomiting, diarrhea, or excessive urination). Alcohol can also make chemotherapy-induced mouth sores worse and increase pain. Alcohol is irritating to the stomach and can aggravate the symptoms of chemotherapy-induced nausea. Alcohol can also interfere with the production of blood cells, potentially worsening bone marrow suppression in people undergoing chemotherapy. The risk is highest among heavy drinkers but can also affect moderate drinkers.
Alcohol can also indirectly impact treatment and a person's ability to cope. It can cause sleep problems, which correspond to poorer survival times in people with advanced cancer. As a depressant, alcohol can also worsen depression and make it harder for people to cope during chemotherapy.
A Day in the Life of a Brewery Worker
You may want to see also

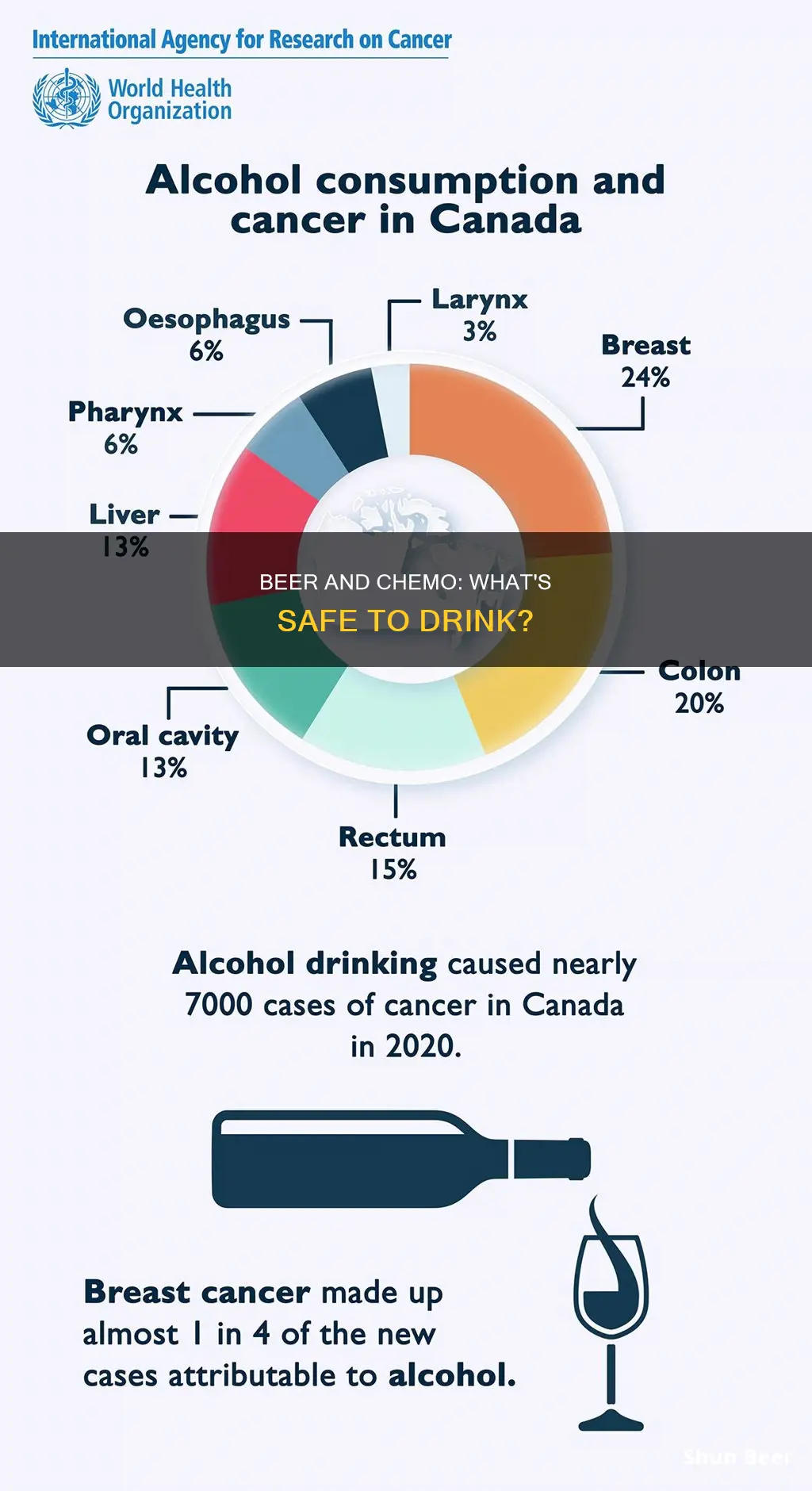
Alcohol increases the risk of cancer recurrence
Alcohol is a known carcinogen that increases the risk of cancer and cancer recurrence. Even drinking small amounts of alcohol increases cancer risk. Alcohol use accounts for about 6% of all cancers and 4% of all cancer deaths in the United States.
When you drink alcohol, the body prioritises breaking it down to get rid of it as quickly as possible. This process creates toxic chemicals and means that the body cannot properly break down and absorb essential nutrients. This results in alcohol increasing cancer risk by:
- Damaging DNA, proteins, and fats in the body
- Decreasing the availability of essential nutrients that can protect against cancer, like vitamins A, C, D, E and the B vitamins
- Increasing estrogen levels in the blood
Alcohol and chemotherapy
Many of the drugs used to treat cancer are broken down by the liver, which is also where alcohol is processed. This can cause liver inflammation, which could impair chemotherapy drug breakdown and increase side effects from treatment. Alcohol can also irritate mouth sores, which chemotherapy patients often experience, or even make them worse.
Alcohol and breast cancer
Drinking even small amounts of alcohol is linked with an increased risk of breast cancer in women. Alcohol can raise estrogen levels in the body, which may explain the increased risk. Avoiding or cutting back on alcohol may be an important way for many women to lower their risk of breast cancer.
Alcohol and other cancers
Alcohol use has been linked with cancers of the mouth, throat, voice box, and oesophagus. Drinking and smoking together raises the risk of these cancers many times more than drinking or smoking alone. This might be because alcohol helps harmful chemicals in tobacco get inside the cells that line the mouth, throat, and oesophagus.
Alcohol has also been linked to an increased risk of liver cancer, as regular, heavy alcohol use can damage the liver, leading to inflammation and scarring. Alcohol use has also been linked with a higher risk of colon and rectal cancer, and there is evidence to suggest it may also increase the risk of stomach, skin, prostate, pancreatic, lung, gallbladder and ovarian cancers.
Antibiotics and Alcohol: Is It Safe to Drink Beer?
You may want to see also
Frequently asked questions
It is advised to consult your doctor before drinking alcohol after chemotherapy. Generally, an occasional beer or glass of wine is unlikely to have serious effects, but some chemotherapy drugs can interact with alcohol and cause side effects such as dehydration, diarrhoea, and mouth sores.
There is no definitive answer to this question, as it depends on the individual's health and the specific chemotherapy treatment they received. It is always best to consult your doctor or healthcare team for personalised advice.
Alcohol is processed by the liver, and so are many chemotherapy medications. Consuming alcohol during chemotherapy can cause additional strain on the liver and worsen side effects such as dehydration, making the treatment harder to tolerate.
Drinking alcohol after chemotherapy can increase the risk of cancer recurrence. Studies have shown that breast cancer survivors who drank more than three to four drinks per week were at a higher risk of cancer returning. Alcohol consumption is also associated with weight gain, which is a known risk factor for cancer.